Multiple Tumor Marker Test Results: Comprehensive Analysis Guide
Multiple Tumor Marker Test Results: Comprehensive Analysis Guide
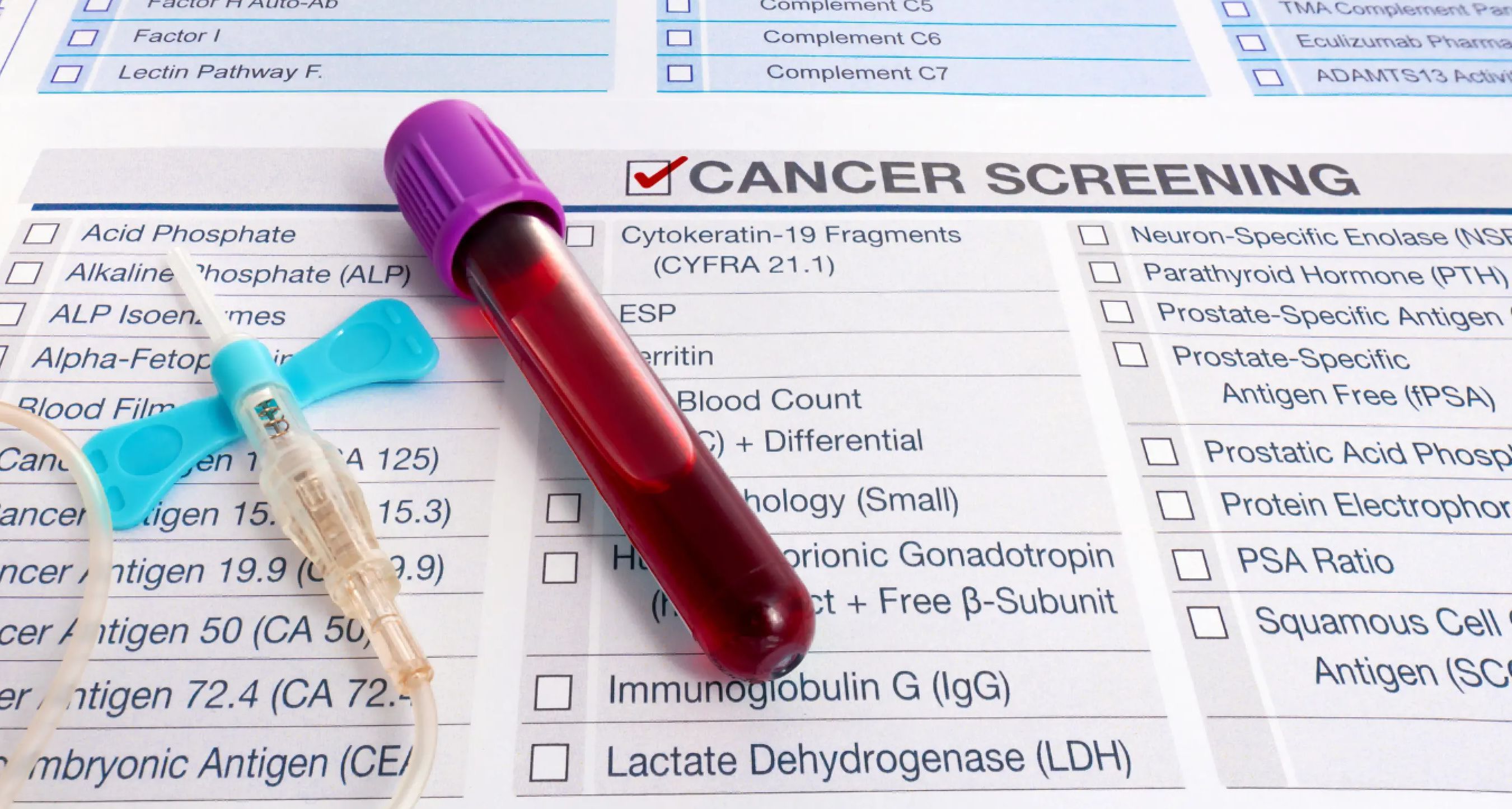
When healthcare providers order cancer panels that test for multiple tumor markers, they aim to create a broader picture of potential disease activity.
While tumor markers provide important clues, they do not function as definitive diagnostic tools on their own.
If you've recently received your results back and need a personalized explanation regarding what they mean, LabAnalyzer can offer a specific breakdown.
Interpreting multiple tumor marker test results requires understanding each marker’s meaning, the combinations that raise concern, and the need for context with imaging, symptoms, and additional testing.
This guide explains how to evaluate cancer panel results, handle mixed results, and plan next steps after receiving abnormal markers.
Common Tumor Marker Combinations
Healthcare providers often order certain tumor markers together because they help evaluate different cancer types or improve diagnostic sensitivity when used in combination.
For pancreatic or biliary cancers, CA 19-9, CEA, and CA 125 are typically tested together. CA 19-9 serves as the primary pancreatic cancer marker. CEA provides additional information for advanced disease, and CA 125 helps evaluate peritoneal spread.
For ovarian cancer, CA 125, HE4, and sometimes CEA are combined. CA 125 serves as the primary ovarian cancer marker. HE4 improves specificity beyond CA 125 alone. Together, they are used in the ROMA score to assess risk.
For testicular cancer, AFP, beta-hCG, and LDH are commonly tested. AFP rises in yolk sac tumors and embryonal carcinoma. Beta-hCG marks choriocarcinoma elements. LDH serves as a general marker of tumor burden and necrosis.
For gastrointestinal cancers, CEA, CA 19-9, and CA 72-4 are combined. CEA is the primary marker for colorectal cancer. CA 19-9 provides information on pancreatic involvement. CA 72-4 improves sensitivity for gastric cancer.
In breast cancer, CA 15-3, CA 27.29, and CEA are measured. CA 15-3 and CA 27.29 track the MUC1 antigen. CEA adds information about potential metastatic spread. These markers are more useful for monitoring than diagnosis.
For liver cancer, AFP and Des-gamma-carboxy prothrombin (DCP) are used. AFP is the primary hepatocellular carcinoma marker, while DCP complements AFP and improves detection rates when used together.
In prostate cancer, PSA and free PSA are evaluated. PSA serves as the primary marker, while free PSA percentage helps distinguish cancer from benign conditions. PSA velocity, the rate of change over time, also provides important information.
Using digital health platforms like LabAnalyzer helps track these multiple values over time, enabling better detection of concerning patterns.
Interpreting Mixed Results
Sometimes one marker shows elevation while others remain normal. Understanding how to interpret this pattern plays an essential role in evaluation.
If a single mild elevation occurs, it often reflects non-cancerous inflammation, infection, or a benign condition. It typically warrants repeat testing after a few weeks. This pattern is most common with non-specific markers like CEA.
When multiple moderate elevations are present, suspicion for cancer or significant inflammation increases. Imaging and possibly biopsy become necessary to clarify findings. The overall pattern often provides more information than individual absolute values.
If an isolated high-risk marker elevation occurs, such as CA 19-9 above 1000 U/mL, AFP above 400 ng/mL, or CA 125 above 1000 U/mL, it strongly suggests malignancy but still requires confirmation with imaging.
Cross-reactivity between conditions complicates interpretation. Many markers rise in multiple cancer types or increase due to inflammation or infection. Liver or kidney dysfunction can affect clearance. Smoking and other lifestyle factors influence baselines.
The stage of disease also affects marker interpretation. Some markers rise only in advanced cancer stages. Early cancers may show minimal or no elevation. Tumor differentiation affects marker production, and some tumors do not produce the expected markers at all.
Mixed tumor marker results require cautious interpretation. Patterns, trends, and clinical correlation matter more than isolated numbers. Digital health tools help organize these complex data sets for better visualization.
Sensitivity and Specificity Factors
Each tumor marker has different levels of sensitivity for detecting disease and specificity for ruling out non-cancer conditions.
Markers with high sensitivity but low specificity, such as CA 125 in endometriosis or CEA in smokers, have more false positives. They are better for monitoring known disease rather than diagnosing it. Higher cutoff values often improve clinical utility.
Markers with high specificity but lower sensitivity, such as CA 19-9 in early pancreatic cancer or AFP in some liver cancers, might miss early cancers but have positive results that are more likely to represent true disease. These are often combined with other markers to improve detection.
For example, CA 125 for ovarian cancer has seventy to eighty percent sensitivity in advanced disease but only fifty percent in early disease, with about eighty percent specificity in postmenopausal women.
CA 19-9 shows seventy to ninety percent sensitivity for pancreatic cancer but lower specificity when biliary disease is present.
CEA demonstrates thirty to forty percent sensitivity in early colorectal cancer and seventy to eighty percent in advanced stages, with ninety percent specificity in healthy non-smokers.
AFP has sixty to eighty percent sensitivity for hepatocellular carcinoma and eighty to ninety percent specificity when liver disease is absent.
PSA demonstrates high sensitivity, although specificity varies with cutoff values.
Beta-hCG shows forty to sixty percent sensitivity for germ cell tumors with over ninety-five percent specificity in men.
No tumor marker achieves perfection, and each requires interpretation alongside clinical findings and imaging. Using digital health platforms facilitates tracking of multiple markers simultaneously.
Follow-up Testing Strategy
When tumor markers show abnormality, follow-up testing becomes critical to clarify the cause and guide next steps.
Confirming the elevation pattern is important. A repeat tumor marker panel is recommended in two to six weeks. Baseline values, if available, should be compared. The trend direction and rate of change need evaluation. Technical or laboratory errors should be ruled out.
Addressing potential non-cancer causes comes next. Healthcare providers should check for infections or inflammations, evaluate organ function such as kidney and liver function, consider medication effects, and assess for benign conditions that can elevate markers.
Targeted imaging is the next step. CT scans provide high-resolution evaluation of potential tumor sites. MRI offers better soft tissue characterization. PET/CT scans detect metabolically active lesions. Ultrasound serves as a first-line evaluation for organs like the thyroid and liver.
Specialized testing may be necessary. Hepatitis panels are important for liver marker elevations. Inflammatory markers like CRP and ESR help assess systemic inflammation. A complete blood count evaluates general health status. Organ-specific function tests further clarify findings.
Tissue assessment is often necessary. Biopsies are performed if imaging reveals a suspicious mass. Liquid biopsy options for circulating tumor DNA are becoming more widely available. Cytology is used for accessible body fluids, and surgical exploration is an option in selected cases.
Persistent or worsening elevations across one or more markers typically move the patient toward imaging and biopsy. Digital health tracking tools help document these changes systematically.
Monitoring Recommendations
Healthcare providers often monitor tumor markers over time, especially after cancer diagnosis confirmation or for recurrence risk tracking.
During active cancer treatment, tumor markers are monitored every one to three months, often before each treatment cycle to assess response. Testing may occur more frequently if treatment decisions depend heavily on marker levels.
After surgery or during remission, markers are typically monitored every three months during the first year, every three to six months during the second year, and every six months for years three through five. Annual monitoring may be sufficient after five years if stability persists.
High-risk individuals without cancer may undergo tumor marker testing every six to twelve months depending on genetic risk factors or strong family history. Monitoring schedules align with imaging surveillance whenever possible.
The benefits of structured monitoring include early detection of recurrence before symptoms, assessment of treatment effectiveness, identification of resistance patterns, guidance for imaging frequency, and reassurance during surveillance periods.
Trend tracking, rather than isolated tests, provides the most meaningful assessment of disease status using tumor markers. Digital platforms like LabAnalyzer help maintain testing schedules and visualize changes over time.
Discussing Results with Your Healthcare Provider
When reviewing multiple tumor marker results, detailed conversations with your healthcare provider become important.
When discussing your specific results, ask which marker or markers show abnormality and by how much. Ask how these values compare to previous results. Inquire whether non-cancerous reasons could explain these elevations. Discuss which cancer types are associated with your pattern. Ask about the reliability of these markers for your situation.
For next steps, ask what further testing your provider recommends and how urgently additional imaging or biopsy is needed. Find out whether marker testing should be repeated and when. Clarify what symptoms should prompt earlier evaluation.
For long-term planning, ask how monitoring will proceed over time. Find out what changes would raise significant concern. Discuss how lifestyle factors may affect tumor marker results. Clarify how these tests integrate with other screenings. Ask about digital tools that can help track results between appointments.
Clear communication ensures you understand your panel results’ implications and actively participate in planning next steps. Digital health platforms support this process by organizing results for productive discussions with healthcare providers.