PSA Doubling Time: What Your Numbers Mean
PSA Doubling Time: What Your Numbers Mean
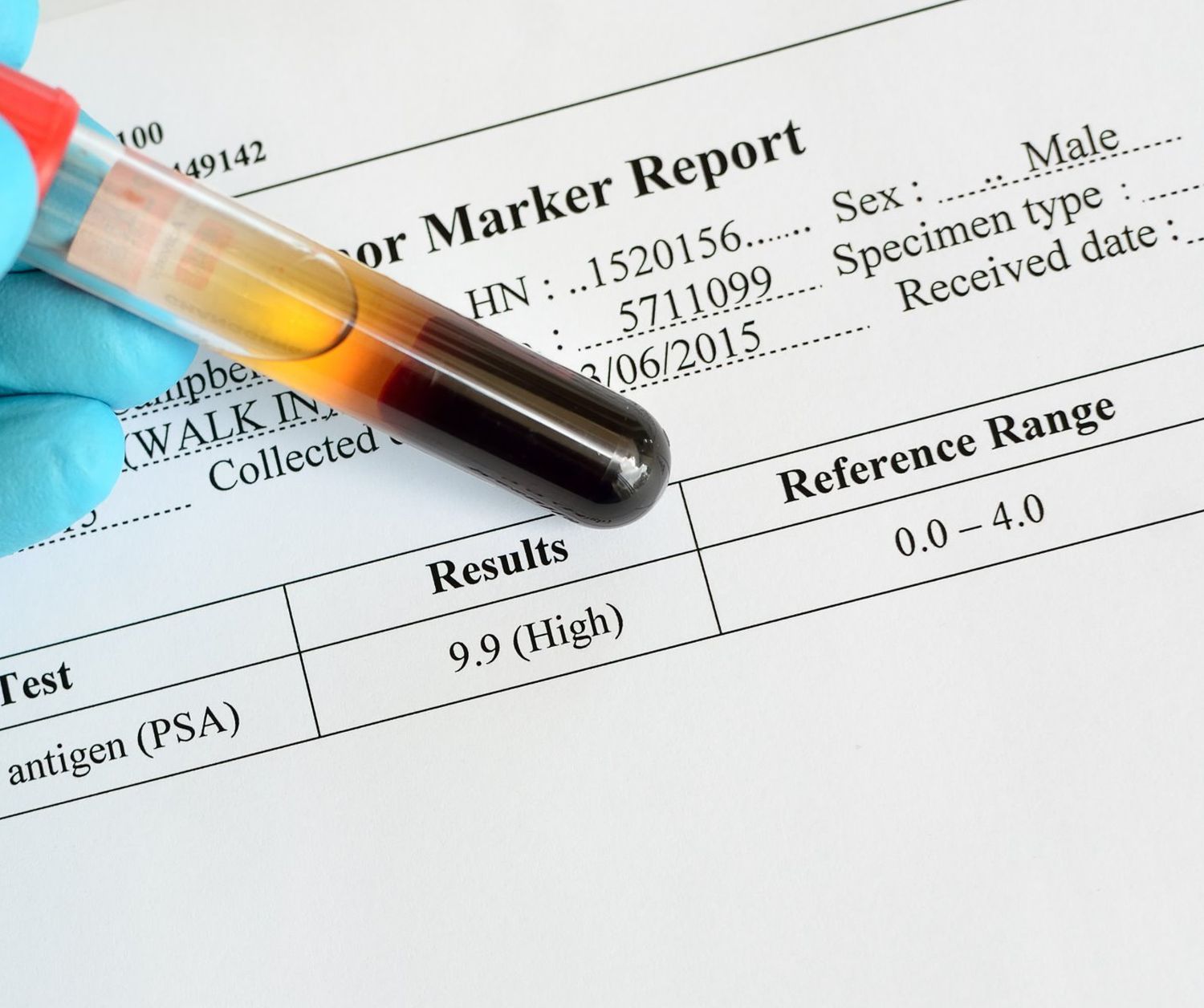
When tracking prostate-specific antigen (PSA) levels, the absolute number holds less importance than how quickly that number changes. PSA doubling time and PSA velocity help healthcare providers evaluate how aggressively prostate issues, including prostate cancer, develop.
If you've recently received your results back and need a personalized explanation regarding what they mean, LabAnalyzer can offer a specific breakdown.
More broadly, this guide explains how to understand PSA doubling time, how to calculate PSA velocity, and how these markers help guide risk assessment, follow-up testing, and treatment decisions.
What PSA Doubling Time Measures
PSA doubling time represents the length of time it takes for your PSA level to double. It offers a dynamic view of disease progression that a single PSA value cannot provide.
A short doubling time suggests faster-growing disease. This pattern indicates more rapid cellular proliferation, often correlates with higher grade cancer, predicts earlier clinical progression, and makes a stronger case for intervention.
A long doubling time indicates slower disease progression. This suggests more indolent disease behavior, allows time for careful monitoring, often supports an active surveillance approach, and creates less urgency for immediate treatment.
Clinically, PSA doubling time predicts cancer aggressiveness in newly diagnosed patients, forecasts recurrence likelihood after surgery or radiation, helps identify patients needing earlier intervention, contributes to overall prognostic assessment, and guides treatment intensity decisions.
Using digital health platforms like LabAnalyzer helps calculate doubling time accurately by tracking PSA values over extended periods.
Calculating Your PSA Velocity
PSA velocity measures how fast PSA levels rise per year, rather than how long they take to double. While slightly different from doubling time, velocity functions as another important risk indicator.
To calculate PSA velocity, subtract the earlier PSA value from the later PSA value, then divide the result by the time interval in years.
For example, if a PSA rises from 2.0 ng/mL to 4.0 ng/mL over two years, the velocity is (4.0 - 2.0) divided by 2, which equals 1.0 ng/mL per year.
When multiple measurements exist, it is best to calculate the change between each consecutive measurement, divide by the time interval, and then average the results for an overall velocity.
General interpretations for PSA velocity are as follows: less than 0.35 ng/mL per year indicates low risk. A range between 0.35 and 0.75 ng/mL per year suggests low-intermediate risk. A velocity between 0.76 and 2.0 ng/mL per year signals intermediate-high risk. A velocity greater than 2.0 ng/mL per year points to a high risk for aggressive disease.
It is important to have at least three measurements separated by three or more months for a reliable calculation. Laboratory variations and PSA fluctuations from non-cancer causes can impact accuracy. Using digital tracking tools improves precision, and consistent testing intervals yield more reliable results.
Both PSA doubling time and PSA velocity should work together to assess progression risk. Digital tracking platforms enable more accurate calculations than mental math or simple spreadsheets.
Risk Assessment by Rate of Change
The speed of PSA changes helps healthcare providers assess whether to observe, investigate further, or begin treatment.
In terms of PSA doubling time risk categories, a doubling time greater than 24 months indicates very low risk and an excellent candidate for active surveillance. A doubling time between 12 and 24 months suggests lower risk and often eligibility for active surveillance. A doubling time between 6 and 12 months represents intermediate risk, suggesting closer monitoring. A doubling time between 3 and 6 months indicates high risk and suggests aggressive disease. A doubling time less than 3 months represents very high risk, with rapid disease progression likely.
Absolute PSA level affects interpretation of doubling time. Higher baseline PSA combined with rapid doubling creates greater concern. Age and comorbidities influence risk tolerance, and family history modifies risk assessment. Previous biopsy results provide additional context. Digital tracking visualizes acceleration or deceleration trends.
Research shows that doubling times less than three months correlate strongly with metastatic progression. Times greater than twelve months rarely associate with cancer-specific mortality within five years. Post-treatment doubling times less than six months predict earlier metastasis. In general, the shorter the doubling time, the higher the Gleason score typically found on biopsy.
A short PSA doubling time strongly predicts aggressive disease and triggers more urgent action. Systematic tracking with digital health tools helps identify concerning changes earlier.
Follow-up Testing Guidelines
When rising PSA levels or concerning velocity or doubling time appear, healthcare providers typically recommend further testing.
To confirm the trend, repeat PSA testing every three to six months. Using the same laboratory ensures consistency. Scheduling testing at similar times of day helps minimize variations. Temporary causes of elevation must be ruled out. Digital tracking helps validate true trends.
Advanced imaging plays an important role. Multiparametric MRI helps look for suspicious lesions and provides a PI-RADS score to assess cancer likelihood. It also guides targeted biopsy if needed and evaluates for extraprostatic extension. MRI also assesses prostate size and structure.
Tissue evaluation often becomes necessary. Standard systematic biopsy samples multiple prostate regions, while MRI-fusion targeted biopsy focuses on suspicious areas. A transperineal approach can reduce infection risk. Extended sampling may be needed for higher-risk scenarios. Molecular testing on tissue samples may also help refine treatment decisions.
Additional biomarkers assist evaluation. The PCA3 urine test measures cancer-specific RNA. The 4Kscore blood test combines four kallikrein markers. The PHI (Prostate Health Index) combines different PSA forms. Other options include SelectMDx or ExoDx urine tests for biopsy decision-making, and genomic tissue tests if prior biopsy confirmed cancer.
Persistent rising PSA, high velocity, or short doubling time should trigger imaging and biopsy discussions. Digital health platforms help maintain testing schedules and document multiple parameters.
When to Consider Treatment
Decisions about moving from monitoring to active treatment depend heavily on PSA trends combined with other clinical factors.
Treatment should be considered if PSA kinetics show concerning patterns. Doubling time falling below six to twelve months, PSA velocity exceeding 2.0 ng/mL per year, acceleration in doubling time, or rapid rise despite relatively low absolute values suggest the need for intervention. Digital tracking can confirm persistent patterns.
Imaging findings also influence treatment decisions. PI-RADS 4-5 lesions on MRI, evidence of extraprostatic extension, seminal vesicle involvement, or growing lesions on serial imaging raise concern. Multiple suspicious regions further support the need for treatment.
Biopsy results also carry significant weight. A Gleason Grade Group of three or higher, a high percentage of positive cores, higher tumor volume in individual cores, and perineural invasion all suggest more aggressive disease requiring treatment.
Patient factors influence timing as well. Younger patients with longer life expectancy, few competing health concerns, strong family history of aggressive disease, or significant anxiety about monitoring might lean toward earlier treatment.
Rapid PSA changes often shift management from active surveillance to definitive treatment like surgery, radiation, or hormone therapy. Digital tracking tools help visualize these changing patterns and facilitate timely intervention decisions.
Monitoring Protocol Options
If immediate treatment is not necessary, ongoing monitoring becomes critical to catch further changes early.
Monitoring guidelines for rising PSA depend on the situation. Low, stable PSA with slow velocity typically warrants PSA testing every six to twelve months. PSA rising moderately, with doubling time greater than twelve months, calls for PSA testing every three to six months plus yearly MRI. PSA rising rapidly, with doubling time less than twelve months, requires PSA testing every three months with prompt imaging or biopsy. Post-treatment rising PSA requires testing every one to three months until a pattern becomes established.
A comprehensive monitoring strategy includes regular laboratory monitoring. This involves regular PSA testing at consistent intervals, consideration of free PSA percentage or PSA density, tracking the post-treatment PSA nadir, maintaining testing even during stable periods, and documenting prostate size changes over time.
Physical examination remains important. Digital rectal exams every six to twelve months help assess prostate consistency, detect nodules or asymmetry, evaluate the seminal vesicle region, and check lymph nodes if needed.
Advanced monitoring tools assist in long-term management. Prostate MRI every one to two years during surveillance provides high sensitivity. PSMA PET scanning becomes important for post-treatment rises. Repeat targeted biopsy is needed for concerning MRI changes. Genomic risk assessment can refine treatment decisions. Digital symptom tracking between appointments supports comprehensive care.
Psychological support remains important. Anxiety related to "watchful waiting" should be addressed, clear intervention triggers should be established, and expectations about the duration of monitoring should be set. Quality of life considerations must be discussed, and access to support resources provided.
Customized monitoring protocols based on PSA kinetics help ensure the right balance between vigilance and avoiding unnecessary procedures. Digital health tracking through platforms like LabAnalyzer helps maintain these complex monitoring schedules and visualize trends over time.